1Part Manager, Department of Nursing, Samsung Medical Center, Korea.
2Professor, College of Nursing, Seoul National University, The Research Institute of Nursing Science, Korea.
Copyright © 2011 Korean Academy of Nursing Administration
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Age; 20-29 vs 30-39, 20-29 vs 40-49, 30-39 vs 40-49, Education; College vs Graduate school, University vs Graduate school, Number of visits to Medical Center; 0 vs 2, 0 vs Above 3
†number(%)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Age; 20-29 vs 40-49, 30-39 vs 40-49, Education; Junior College vs Graduate school, Current Work Experience; <1 vs ≥3, Working Unit; ICU vs OPD & Others, Number of visits to Medical Center; 0 vs 2
†number(%)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Number of visits to Medical Center; 0 vs 2
†number(%)
(1) ICU; Intensive Care Unit (2) OR & PAR; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): SF-36 Total score-Number of visits to Medical Center; 0 vs 1, 0 vs 2, 0 vs Above 3, 1 vs Above 3, PCS-Number of visits to Medical Center; 0 vs 1, 0 vs 2, 0 vs Above 3, 1 vs Above 3, MCS-Current Work Experience; <1 vs ≥3

General Characteristics of Participants (n=401)
(1) ICU; Intensive Care Unit, (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit
(3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care
(5) SOC; Sense of Coherence
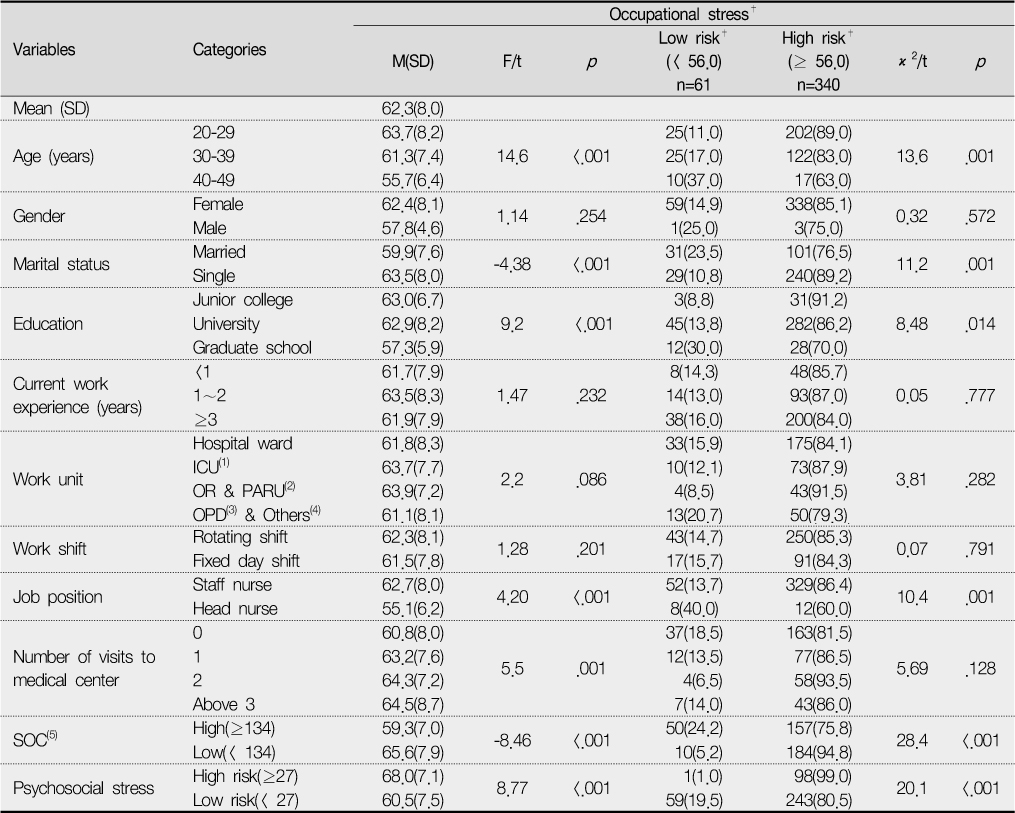
Occupational Stress According to General Characteristics, SOC and Psychosocial Stress (continued) (n=401)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Age; 20-29 vs 30-39, 20-29 vs 40-49, 30-39 vs 40-49, Education; College vs Graduate school, University vs Graduate school, Number of visits to Medical Center; 0 vs 2, 0 vs Above 3
†number(%)
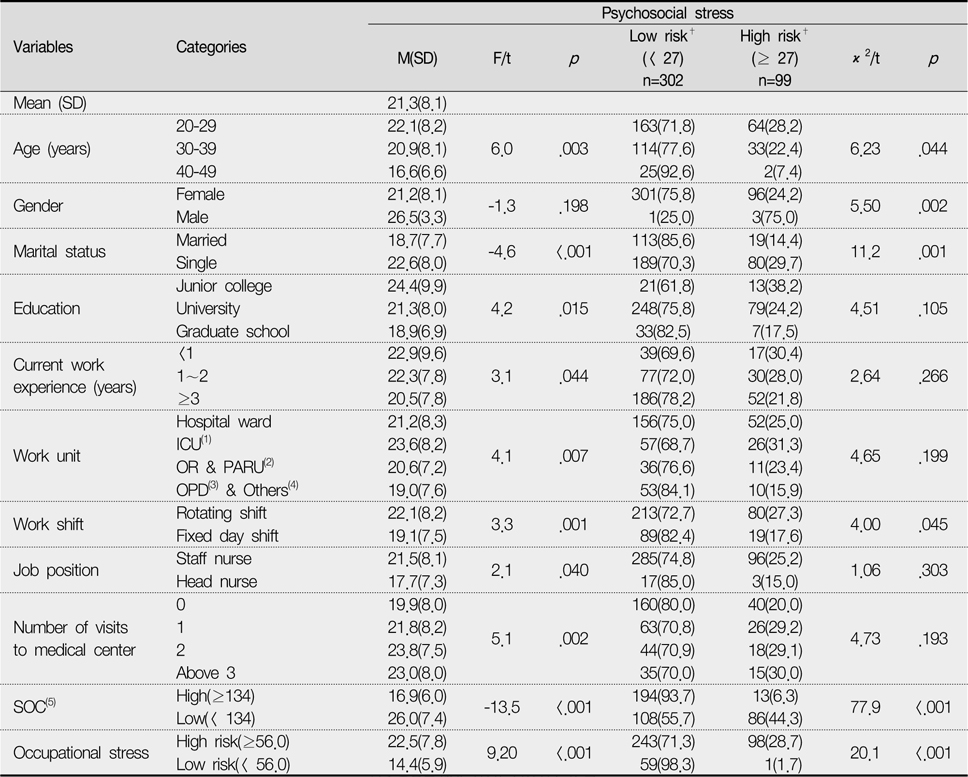
Psychosocial Stress According to General Characteristics, SOC and Occupational Stress (n=401)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Age; 20-29 vs 40-49, 30-39 vs 40-49, Education; Junior College vs Graduate school, Current Work Experience; <1 vs ≥3, Working Unit; ICU vs OPD & Others, Number of visits to Medical Center; 0 vs 2
†number(%)
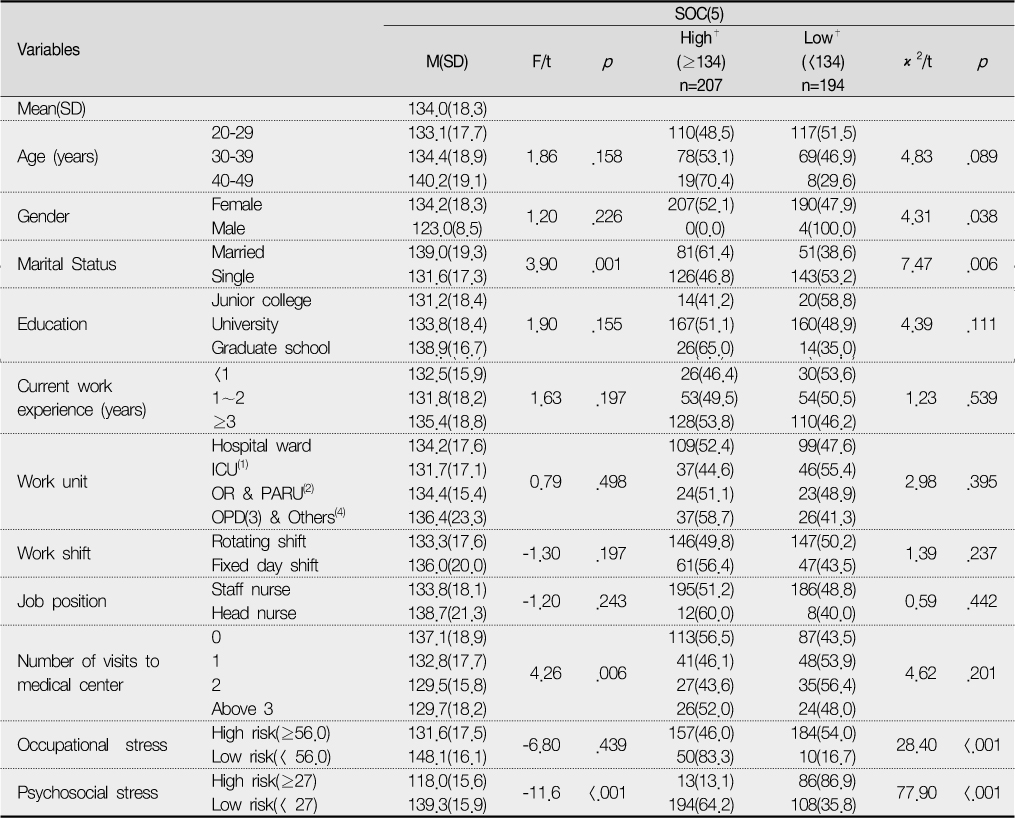
SOC According to General Characteristics and Stress (n=401)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Number of visits to Medical Center; 0 vs 2
†number(%)
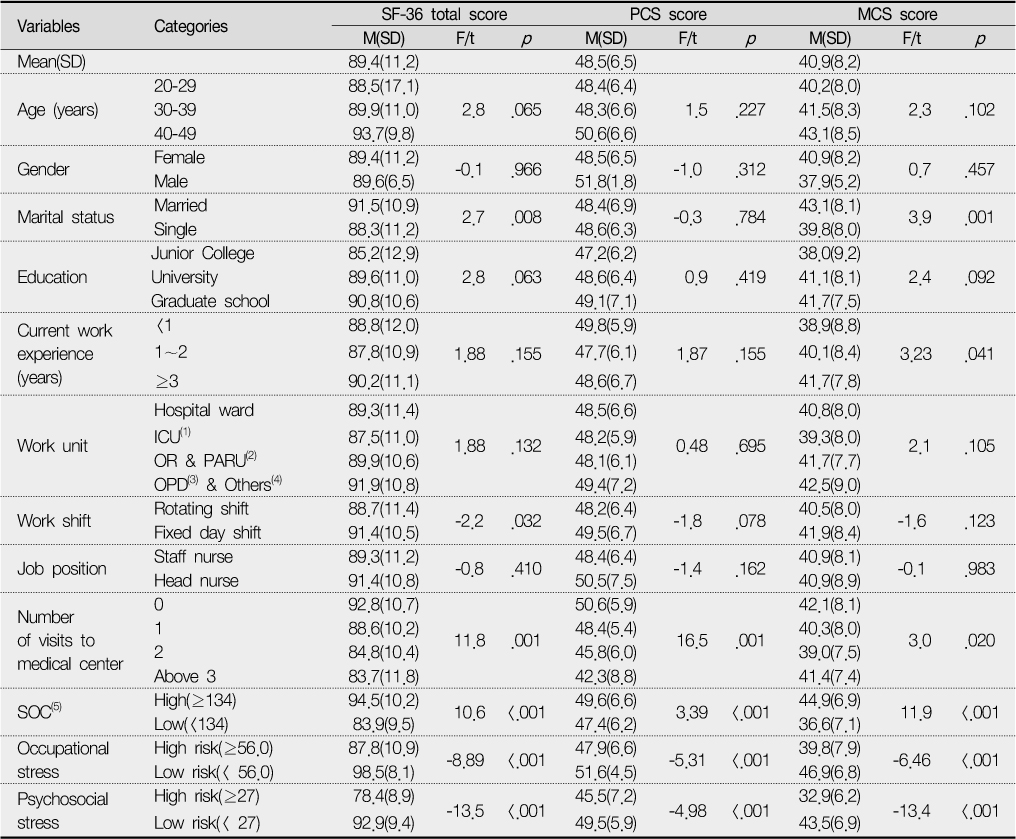
SF-36 Total Score, PCS Score and MCS Score According to General Characteristics, SOC and Stress (n=401)
(1) ICU; Intensive Care Unit (2) OR & PAR; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
*Bonferroni multiple comparisons test for Continuous variables(p-value<.05): SF-36 Total score-Number of visits to Medical Center; 0 vs 1, 0 vs 2, 0 vs Above 3, 1 vs Above 3, PCS-Number of visits to Medical Center; 0 vs 1, 0 vs 2, 0 vs Above 3, 1 vs Above 3, MCS-Current Work Experience; <1 vs ≥3
Correlation Analysis of SOC, SF-36 Total Score, PCS Score, MCS Score and Stress
*P< .05 **P<.01
(1) SOC; Sense of Coherence
(2) PCS; Physical Component Summary
(3) MCS; Mental Component Summary
Multiple Linear Regression Analysis for SOC and sSress
(1) SOC; Sense of Coherence
Multiple Linear Regression Analysis for SF-36 Total Score, PCS Score and MCS Score
(1) SOC; Sense of Coherence
(2) PCS; Physical Component Summary
(3) MCS; Mental Component Summary
(1) ICU; Intensive Care Unit, (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence *Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Age; 20-29 vs 30-39, 20-29 vs 40-49, 30-39 vs 40-49, Education; College vs Graduate school, University vs Graduate school, Number of visits to Medical Center; 0 vs 2, 0 vs Above 3 †number(%)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence *Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Age; 20-29 vs 40-49, 30-39 vs 40-49, Education; Junior College vs Graduate school, Current Work Experience; <1 vs ≥3, Working Unit; ICU vs OPD & Others, Number of visits to Medical Center; 0 vs 2 †number(%)
(1) ICU; Intensive Care Unit (2) OR & PARU; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence *Bonferroni multiple comparisons test for Continuous variables(p-value<.05): Number of visits to Medical Center; 0 vs 2 †number(%)
(1) ICU; Intensive Care Unit (2) OR & PAR; Operating Room & Postanesthetic Recovery Unit (3) OPD; Outpatient Department (4) Others; Dialysis room, Intravenous injection team & Home care (5) SOC; Sense of Coherence *Bonferroni multiple comparisons test for Continuous variables(p-value<.05): SF-36 Total score-Number of visits to Medical Center; 0 vs 1, 0 vs 2, 0 vs Above 3, 1 vs Above 3, PCS-Number of visits to Medical Center; 0 vs 1, 0 vs 2, 0 vs Above 3, 1 vs Above 3, MCS-Current Work Experience; <1 vs ≥3
*P< .05 **P<.01 (1) SOC; Sense of Coherence (2) PCS; Physical Component Summary (3) MCS; Mental Component Summary
(1) SOC; Sense of Coherence
(1) SOC; Sense of Coherence (2) PCS; Physical Component Summary (3) MCS; Mental Component Summary

