Abstract
-
Purpose
This study explored the literature on non-value-added (NVA) activities and non-nursing tasks (NNT). We analyzed domestic and international research trends and examined the types and characteristics of nursing tasks to improve efficiency.
-
Methods
A comprehensive literature search was conducted using RISS, DBpia, PubMed, CINAHL, Medline, and Embase. Relevant studies published up to 2024 were identified using keywords such as “non-value-added activity,” “non-value-added nursing activity,” “non-nursing tasks,” and “nursing.”
-
Results
Analysis of 25 studies revealed that 11 studies focused on NVA activity and 14 on NNT. Direct nursing tasks were classified into eight categories; indirect tasks were classified into seven categories. NVA activities were grouped into five main categories: “personal,” “waste,” “documentation,” “necessary activities,” and “unit-related,” with overlapping subcategories such as “interruption” and “duplicating.” Similarly, NNT were categorized into eight types, including “admission,” “equipment,” and “administrative activities.” Although conceptually distinct, NVA activities and NNT often overlap. Reducing tasks unrelated to essential nursing care significantly improves job satisfaction, patient outcomes, and work efficiency. These findings provide valuable insights for optimizing nursing workflows and enhancing the quality of care.
-
Conclusion
Identifying and reducing NVA activities and NNT enhance nursing efficiency and provide foundational data for improving clinical practice and patient safety.
-
Key Words: Workload; Efficiency, Organizational; Time management; Scoping review
-
주요어: 간호활동, 업무, 주제범위 문헌고찰
서 론
1. 연구의 필요성
2017년부터 시작된 건강보험심사평가원의 환자 경험 평가 항목은 간호사, 의사, 투약 및 치료과정, 병원 환경, 환자권리보장, 전반적인 평가의 총 6개의 영역으로 구성되었으며, 이 중 간호사 영역이 환자 경험에 가장 큰 영향을 미치는 것으로 나타났다[
1]. 간호사는 환자의 간호뿐만 아니라 환자 치료 계획 수립과 평가에 적극적으로 참여하여 환자 치료에 직접적으로 영향을 미치고 있고, 의료 서비스를 제공하는 간호사의 역할과 영역이 지속적으로 확대되고 강화되어 병원 의료 서비스의 핵심적인 구성 요소로 작용하고 있다[
1]. 그러나 의료기관에서는 간호사의 인적 자원이 제한되어 있음에도 불구하고, 간호사의 업무량은 꾸준히 증가하고 있다. 이와 같은 상황에서 업무 범위에 관한 규정이 명확히 제시되지 않고 있으며, 관련된 양적 데이터나 연구가 부족한 실정이다. 결과적으로 이는 간호사의 역할 혼선과 직무 만족도 저하를 초래하며, 결과적으로 환자의 간호 질이 저하될 우려가 크다[
2-
4]. 따라서 간호사의 업무 범위를 체계적으로 재정의하고, 명확한 규정을 마련할 필요가 있다. 더욱이, 2024년 의과대학 정원 확대 지침에 따른 전공의 대규모 파업 및 사직, 의료 서비스 중단 초래, 전담/전문간호사 제도 확대와 같은 의료정책의 변화로 인해 의료기관의 재정 악화, 병상 가동률 저하, 의료서비스 전반에 대한 비용 절감 압박으로 인해 간호사의 업무 변화가 가속화되고, 간호사의 업무 부담 증가 및 역할 경계가 모호해지고 있다. 더불어 의료 현장 변화에 따른 간호 업무 요구도가 높아지면서 간호사의 업무 강도는 점차 증가하고 복잡해져, 간호사의 보조적 업무 또한 가중되어 간호 업무의 효율성이 저하된다[
3-
6].
이러한 배경에서 의료 현장은 환자의 안전과 효율성을 모두 추구하기 위해, 병원 경영에 1950년대에 개발된 토요타 생산 시스템(Toyota Production System)의 생산 방법론 중 하나인 린 생산(Lean Manufacturing) 혹은 린 사고(Lean Thinking)를 도입하기 시작하였다[
5]. 린 생산의 핵심 가치는 낭비를 최소화하고 가치를 극대화하여 생산성과 효율성을 향상하고, 궁극적으로 환자 경험과 만족도를 높이는 것이다[
7]. 특히, 환자 경험 및 만족도를 향상하기 위한 전략으로 Ohno [
8]가 제시한 비부가가치 활동(non-value-added activity, NVA activity) 유형이 의료 시스템에 적용되었고, 이를 기반으로 의료기관의 질 향상 활동이 진행되고 있다. 특별히 간호 업무의 효율성을 높이기 위한 방안으로 NVA 활동에 관심이 집중되고 있으며, NVA 활동과 관련된 간호 업무의 유형 및 발생 원인을 분석하거나[
2], NVA 활동 개선을 통한 간호 업무 효율성 향상에 관한 연구가 활발히 시도되었다[
2,
9-
12]. NVA 활동은 반복적이거나 중복되는 업무, 찾기 등 간호사가 임상 실무에서 환자에게 직접적인 생명적 위험을 주지 않는 중요도가 낮은 업무를 의미한다[
2]. 이는 의료진 간의 의사소통, 투약 준비, 간호일지 작성 등을 통해 환자에게 직접적인 치료에 영향을 주지는 않지만 치료 결과에 영향을 주는 간접 간호와는 차이가 있다. 다시 말해 간접 간호가 환자의 질과 안전을 유지하기 위해 필요한 업무라면, NVA 활동은 환자의 치료나 결과에 직접적인 결과에 영향을 미치지 않는 활동이다. 또한 비부가가치 간호 활동(non-value-added nursing activity, NVANA)이라고 명명하기도 하며, 간접 간호 활동과는 다른 습관적으로 이루어지는 간호 업무 중 부가가치가 낮은 활동이지만 개선되지 않아 여전히 임상 실무에서 간호 업무 시간을 단축하지 못하는 사례를 지칭한다[
2,
9]. Storfjell 등[
10]의 연구에 따르면, 간호사들의 전체 근무 시간 중 44%가 직접 간호에 사용되고, 36%가 NVA 활동에 소요되는 것으로 나타났다[
10]. NVA 활동으로는 입∙퇴원 관련 업무, 물품 관리, 검사 관련 업무 등이 이에 해당하며[
12], 재입원 환자에게 동일한 내용의 입원 생활 안내를 제공하거나, 침상 카드를 출력하고 꽂는 업무, 정규적으로 반복되는 물품 인수인계 등 직접 간호 외의 불필요한 시간 소모를 초래하여 간호 업무 효율성을 저해하는 요인으로 작용하고 있다[
9].
이와 같은 비부가가치 간호 활동이나 간호 업무의 경계가 불분명하고 지속적으로 개선되지 않고 반복된다면 환자 안전 및 간호의 질에 부정적인 영향을 미치는 것으로 나타났다[
3,
4,
13,
14]. 이에 임상 간호 실무에서는 직∙간접 간호뿐만 아니라 비간호업무(non-nursing task, NNT)가 문제점으로 지적되고 있다[
4]. NNT는 전문적인 간호 훈련이 필요하지 않은 업무로 문서 출력, 준비, 전화 받기, 병원 물품 및 병실 청결, 물품 정리, 찾기, 샘플 접수 등과 같은 업무가 이에 속한다. NNT는 간호 업무의 본질에서 벗어난 활동으로, 간호 업무 간의 역할 혼동을 일으켜, 간호사들이 본래의 중요한 간호 업무를 제대로 수행하지 못하게 하며, 간호소진 증가[
15]와 업무 효율성을 저하한다[
4,
16]. 이러한 상황은 약물 사용 오류, 낙상, 병원 내 감염 및 욕창 발생 등 환자의 안전을 위협하는 요소로 작용하며, 궁극적으로 환자 맞춤형 치료와 환자 중심 간호의 질을 저해하는 결과를 초래한다[
4,
16]. 또한, NNT를 간호사의 책임으로 간주하는 경우, 현장에서 간호사들이 NNT 수행으로 인한 신체적•정신적 스트레스를 겪게 되며, 이는 직업 만족도와 삶의 질에 부정적인 영향을 미칠 수 있다[
4]. 따라서 NNT 문제를 체계적으로 분석하고 이를 개선하는 것이 중요하며, 명확한 직무 범위를 설정하여 간호사가 환자 간호에 집중할 수 있도록 업무 프로세스를 개선, 적절한 지원과 자원을 제공할 필요가 있다.
결론적으로 NVA 활동과 NNT는 각각의 개념적 차이는 존재하지만, 간호사의 업무 효율성에 있어서 모두 비효율성을 유발하는 요소로 작용한다는 점에서 유사하다. 그러나 현재 간호 업무에 대한 구체적이고 체계적인 근거가 충분하지 않아, 지속적인 간호 업무의 평가와 심층적인 분석이 요구된다. 이를 통해 업무 효율성을 개선하고 간호사의 본질적 역할을 강화하는 방안을 마련할 필요가 있다.
2. 연구의 목적
본 연구는 간호 업무 효율성과 관련된 간호 업무 중 NVA 활동과 NNT에 대한 문헌을 탐색하고, 향후 임상간호 실무 개선을 위한 기초 자료를 제공하기 위함이다. 구체적인 연구의 목적은 다음과 같다.
•NVA 활동과 NNT에 대한 국내외 문헌의 일반적 특성을 분석한다.
•탐색된 문헌에서 언급된 직•간접 간호 업무와 NVA 활동 및 NNT 유형을 분석한다.
•NVA 활동과 NNT의 업무에 대한 특성을 분석한다.
•NVA 활동, NNT의 업무와 간호 업무 효율성에 대하여 분석한다.
3. 용어 정의
∙ 비부가가치 활동(NVA activity): 직접 ∙ 간접 간호 업무 중 환자에게 직접적인 가치를 제공하지 않는 활동을 의미한다[A2]. 이러한 활동은 간호사의 일상 업무에서 상당한 비중을 차지하며, 업무 효율성을 저하하는 요인으로 작용할 수 있고, 업무 유형에 따라 반복적이며 중복되거나, 기다림, 찾기 업무 등을 말한다[A7].
∙ 비간호업무(NNT): 간호사의 업무 범위에 속하지 않는 업무로[
17], 전문적인 간호 훈련이 필요하지 않고, 다른 직원에게 할당 또는 위임할 수 있으며, 간호 업무 책임에서 제외되는 업무이다[
18].
연구방법
1. 연구 설계
본 연구에서는 간호 업무 효율성과 관련된 NVA 활동과 NNT에 대한 주제범위 문헌고찰(scoping review) 연구이며, Arksey와 O’Malley [
19]가 제시한 주제범위 문헌 고찰 5단계 방법론적 기틀과 PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) [
20]을 기반으로 연구의 자료를 수집하였다.
1) 1단계: 연구 문제 설정
본 연구는 연구의 시작에 앞서 상급종합병원 외래 및 병동과 같은 간호 단위에서 간호 업무의 유형과 간호 업무 효율성 향상을 위한 방안을 고찰하였다. 이를 통해 본 연구는 다음의 연구 질문을 도출하였다. 첫째, “현재까지 직접∙간접 간호 이외에 수행되고 있는 NVA 활동 및 NNT는 무엇인가?” 둘째, “이와 관련된 기존 학술지 연구의 동향은 어떠한가?” 셋째, “NVA 활동 및 NNT와 연관된 유사 연구들은 어떠한 내용을 다루고 있는가?” 마지막으로, “이와 같은 NVA 활동 및 NNT의 개선이 간호 업무의 효율성 증진에 어떠한 영향을 미치는가?” 이에 따라 본 연구는 국내∙외 간호학 분야의 연구 동향을 분석하여 간호 업무의 효율성 제고 방안을 모색하고자 한다.
2) 2단계: 관련 연구 검색 및 확인
본 연구에서는 1999년부터 2024년까지 NVA 활동과 NNT와 관련된 문헌을 수집하였다. 문헌 자료 수집은 국내 문헌의 경우 학술연구정보서비스(RISS)와 학술데이터베이스서비스(DBpia)를 활용하였으며, 국외 문헌의 경우 PubMed, CINAHL, Medline, Embase를 이용하였다. 본 연구에서는 Google Scholar, OpenGrey, NTIS 등의 회색문헌(grey literature) 데이터베이스는 제외하였다. 국내외 연구 문헌 탐색을 위해 주요어로 ‘non-value added activity,’ ‘non-value added nursing activity,’ ‘non-nursing tasks,’ ‘nursing’을 조합하여 검색을 수행하였다.
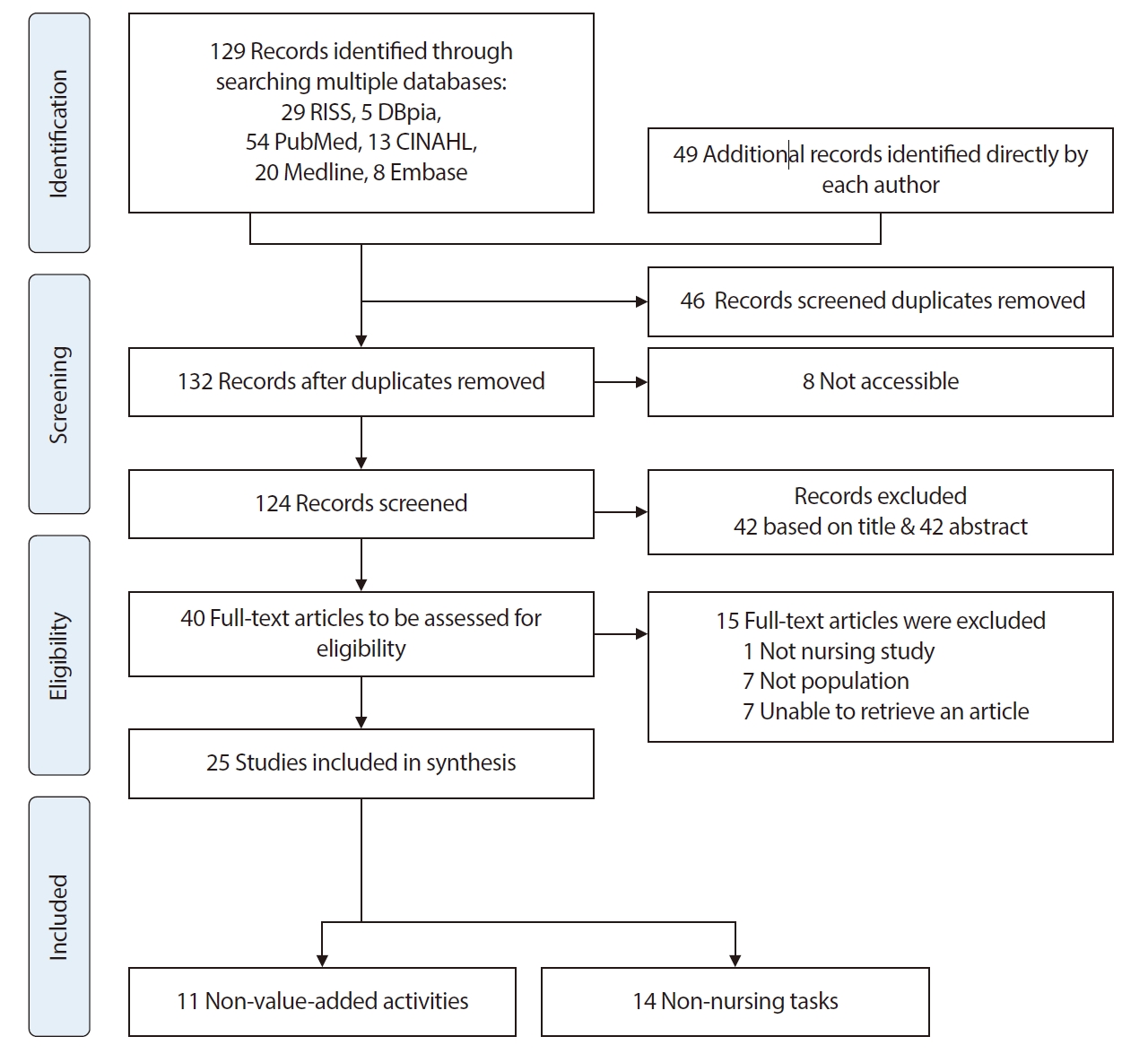
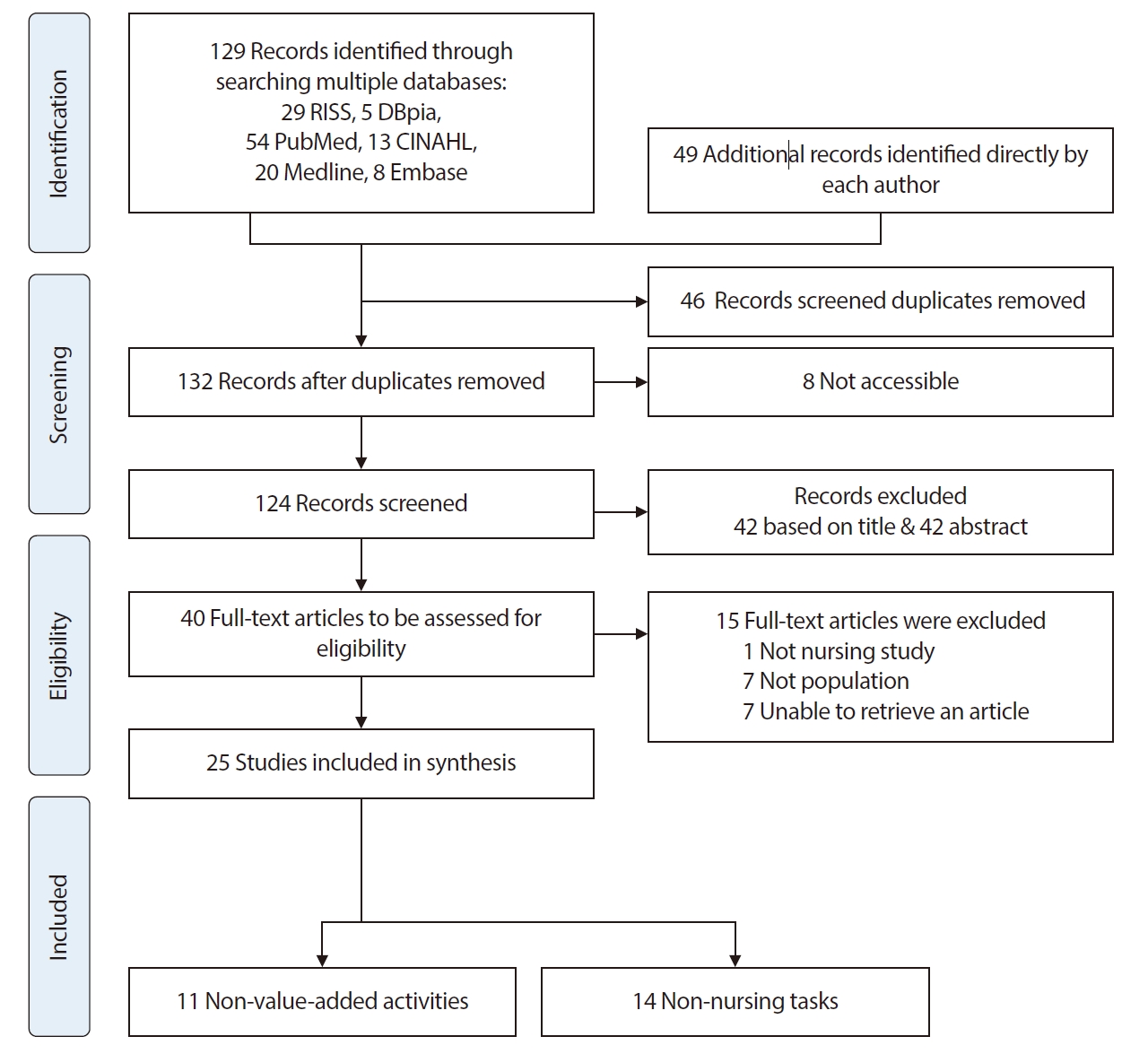
문헌 검색은 총 12명의 연구자가 참여하였다. 각 연구자는 담당 연도를 기준에 따라 2024년 4월 1일부터 4월 10일까지 국내 데이터베이스를 1차 문헌 검색을 시행하였고, 2024년 4월 15일부터 5월 11일까지 국외 데이터베이스를 통해 1차 문헌 검색을 시행하였다. 이를 통해 총 129편의 문헌이 검색되었다. 아울러 검색된 문헌 외에 본 연구 주제와 관련성이 높은 문헌의 누락을 방지하고자 2024년 5월 20일부터 6월 1일까지 국내∙외 데이터베이스를 통해 2차 문헌 검색을 시행하였다. 2차 검색결과 49편의 문헌이 추가로 검색되었다. 이에 총 178편의 문헌을 검색하였고, 중복된 문헌 46편, 본 연구와 무관하거나 접근이 어려운 문헌 8편을 제외하였다. 결과적으로 문헌 검색 및 확인을 통해 132편의 문헌이 검색되었다(
Figure 1).
3) 3단계: 문헌 선정
•문헌 선정: 본 연구의 문헌 선정 과정은 PRISMA-ScR [
20], The PRISMA 2020 statement [
21]와 PICO (Population, Intervention, Comparison, Outcome) 가이드라인[
22]을 근거로 하여 진행하였다. 문헌 선정을 위해 현재까지 발표된 국내∙외 간호 문헌 중 NVA 활동과 NNT 관련 문헌이나 유사 문헌 또는NVA 활동이나 NNT를 통해 간호 업무 효율성과 관련된 문헌을 선정하고자 하였다. 문헌 선정 과정에서는 연구자 2인이 한 조가 되어 각자 독립적으로 담당 연도의 문헌을 검토하여 문헌을 선정하였다. 먼저 문헌의 제목을 검토하여 본 연구와 관련이 없는 42편을 제외하였고, 이후 문헌의 초록을 검토하여 42편의 문헌을 제외하였다. 이에 총 84편의 문헌이 제외되어 40편의 문헌이 선정되었다. 선정된 40편의 문헌 중 간호학과 관련이 없는 1편, 연구 대상과 부합하지 않는 7편, 각 문헌의 초록 및 연구 내용을 재검토한 후 연구자들의 논의와 검토를 거쳐 7편의 문헌을 제외하였다. 본 과정을 통해 최종적으로 25편의 문헌이 본 연구의 연구 대상 문헌으로 선정되었다. 이중 NVA 활동과 관련된 문헌은 11편, NNT와 관련된 문헌은 14편이었다(
Figure 1).
•배제기준: 본 연구에서는 박사학위논문, 학술대회 발표자료, 보고서, 단행본 등과 같은 회색문헌은 제외하였다.
4) 4단계: 자료 기록 및 분석
수집된 문헌 자료는 주제, 초록, 결과 등을 체계적으로 분석하기 위해 Microsoft Excel Microsoft 365용 2024 프로그램을 기반으로 분석 틀을 구축하였다. 각 문헌은 저자, 투고 연도, 연구 수행 국가, 논문 제목, 연구의 주제와 목적, 논문 유형, 연구 방법과 설계, 대상자, 그리고 본 연구의 분석으로 도출된 특정 범주로 세분화하여 기입하고 분석하였다. 또한, 문헌별 NVA 활동, NNT 및 간호 업무 효율성을 비교∙ 분석하기 위해 Zepeda-Lugo 등[
23]의 분석표를 참고하여 본 연구에 맞게 재구성하였다. 아울러 본 연구에서는 문헌 분석 과정을 통해 각 문헌에서 제시된 직접 간호, 간접간호, NVA 활동과 NNT를 통합하여 재분류하였다.
5) 5단계: 자료 결과 분석 및 보고
1~4단계를 통해 수집된 자료는 기술적 통계를 사용하여 분석하였고, 수집된 자료를 분석한 결과는 연구 결과에 제시하였다.
연구결과
1. 탐색된 문헌의 일반적 특성
1) 출판 투고 연도
본 연구에서 분석된 25편의 연구 논문은 1999년부터 2024년 사이에 출판되었다. 이 중 NVA 활동과 관련된 11편은 1999년부터 2022년 사이에, NNT와 관련된 14편은 2003년부터 2024년 사이에 출판되었다. 특히 NVA 활동과 관련된 연구 논문을 살펴보면, 2005년부터 2009년 사이에 4편, 2010년부터 2014년사이에 3편이 집중적으로 출판되었다. 반면, NNT와 관련된 연구 논문은 2015년부터 2019년 사이에 4편이 출판되었으며, 2020년부터 2024년 사이에 5편으로 가장 많은 논문이 출판되었다.
2) 연구 설계
NVA 활동 관련된 연구는 총 11편이며, 그 중 양적 연구 5편[A3,A5,A7,A10,A11], 혼합 연구 4편[A2,A4,A6,A8]으로 나타났다. NNT 관련 연구로는 총 14편이며, 양적 연구 9편[A14-19,A22-24]이 다수를 이루었고, 질적 연구 2편[A20,A25], 문헌 고찰 2편[A12,13], 혼합 연구 1편[A21]으로 나타났다.
3) 연구 수행 국가
연구 수행 국가를 분석한 결과, NVA 활동과 관련된 논문에서는 미국이 6편(54.5%) [A1-6]으로 가장 많았으며, 한국은 4편(36.4%) [A7-9,A11]으로 나타났다. 반면, NNT와 관련된 논문에서는 미국과 한국을 제외한 국가에서 수행된 논문이 10편(71.4%) [A12,A14-17,A20-23,A25]으로 나타났다.
4) 연구 대상
내•외과 병동 대상 연구가 54.4%(12편)로 가장 많았으며[A3-5,A7-9,A15-19,A23], 그 외에 외과 병동[A14,A21], 신경내·외과 병동[A2], 외래[A11]와 분만장, 중환자실, 간호·간병통합서비스 병동[A6,A10,A20,A22,A24,A25] 등이 포함되었다. 또한, 전문간호사[A17], 외래간호사[A11], 간호 보조 직종[A2,A5,A10,A20]을 포함한 연구도 있었다.
2. 직 ∙ 간접 간호 업무, NVA 활동 및 NNT의 유형
본 연구에서는 각 논문에 기술된 NVA 활동과 NNT의 업무 유형을 분석하는 과정에서 직접 간호와 간접 간호 업무의 유형을 함께 분석하였다. 분석 과정을 통해 각 간호 업무를 목록화하기 위해, 각 간호 업무의 고유 유형과 중복된 업무들을 재검토고, 각 업무를 통합하였다. 그 결과, 부가가치 활동의 직∙간접 간호 업무, 비부가가치 활동, 비간호 업무로 재분류 되었다(
Table 2). 부가가치 활동에는 직접 간호 업무 8개, 간접 간호 업무 7개의 항목으로 분류되었다. 비부가가치 활동에는 5개의 업무 유형으로 분류되었고, ‘인력 관련’ 업무를 제외한 4개의 업무는 그 형태에 따라 ‘업무 방해,’ ‘찾기,’ ‘차용,’ ‘기다림,’ ‘업무 중단 후 다시 시작,’ ‘전달,’ ‘반복,’ ‘중복,’ ‘타분야 업무대행’ 9개로 세분화되었다. 마지막으로, NNT와 관련된 업무는 입원∙ 퇴원, ‘물품장비,’ ‘기록(문서)관련,’ ‘낭비,’ ‘행정 업무,’ ‘업무 대행,’ ‘청결,’ ‘기타’ 8개의 업무 유형으로 분류되었다.
분석 결과, NVA 활동과 NNT 중 기록(문서)과 입∙퇴원 과정에서 업무가 중복되며 유사한 것으로 나타났다. 즉, 기록(문서) 작업, 입원과 퇴원 과정에서 처리되는 업무가 부분적으로 중복되거나 중첩되는 것으로 나타났다. 또한, NVA의 낭비 업무는 NNT의 낭비 및 물품장비 관리 업무와 부서 관련 행정 및 청결 업무는 NNT의 행정 업무 및 청결 업무와 유사하거나 중첩되는 부분이 많은 것으로 나타났다. 한편, NNT의 타분야 업무대행과 기타 항목은 NVA 활동보다 간접 간호 업무와 더 유사한 것으로 나타났다. 결과적으로 NVA 활동과 NNT는 범위와 유형에 매우 유사하며, NNT가 NVA 활동의 하위 범주에 속하거나 두 개념의 업무 범위가 명확하게 구분되지 않아 경계가 모호하고 상호 중첩되는 부분이 많았다.
4. NVA 활동, NNT 및 간호 업무 효율성
본 연구에서는 각 논문을 통해 제시된 직•간접 간호 활동, NVA 활동 및 NNT에 소요되는 시간과 간호사의 직무 만족도 등의 결과를 간호 업무 효율성으로 분석하였다(
Table 3). 분석 결과, Capuano 등[A2], Upenieks 등[A3], Desjardins 등[A14], Park 등[A9]의 연구가 간호 단위별 개선 활동 및 업무 효율성을 다루고 있음을 확인하였다. Capuano 등#x0005b;A2]의 연구에서는 간호사의 직접 간호 시간 비율이 5.6%, 개인 활동 시간 비율이 9% 감소하였고, 간접 간호 활동 시간 비율이 8%로 증가한 것으로 나타났다. 이는 간호사가 환자의 퇴원계획, 치료 단계 준비, 간호 조정 활동과 같은 업무의 증가로 인해 직접 간호 활동에 할애할 시간이 줄어든 것이라고 보았다. 또한 간호사는 환자 돌봄 외에 의사소통, 문서 작업, 물품 장비와 같은 활동에 더 많은 시간을 할애하고 있는 것으로 나타났다. 반면, NVA 개선 활동을 통해 technical partner의 직접 간호 활동 시간 비율은 8.7% 증가하였고, support partner의 업무 활동 시간 비율은 26%로 증가하며 직접 간호는 16.13%, 개인 활동 12.32%로 감소한 것으로 나타났다. 또한 입원 및 전원 문서 업무의 대한 프로세스 개선으로 인해 administrative partner의 업무 활동 시간 비율이 16.9%로 감소한 것으로 나타났다. 이와 함께 간호사의 직무 만족도는 52.1점에서 58.7점으로, 간호 관리에 대한 만족도는 52.2점에서 62.1점으로 각각 상승하여 전반적인 직무 만족도가 개선되었다. Upenieks 등[A3]의 연구에 따르면, 간호사의 직접 간호 시간은 25%~31%에 불과하며, 나머지 시간은 간접 간호와 NVA 활동에 사용된다. 특히 환자의 중증도가 높을수록 간접 간호 시간이 증가하였다. Desjardins 등[A14]의 연구에서는 교대 근무 간호사의 직∙간접 시간을 측정한 결과, 직접 간호는 32.8%, 간접 간호는 55.7%, 비간호업무는 9.0%, 개인 활동은 2.5%를 차지하였다. 연구는 의사 소통 프로세스와 간호 보고서 간소화를 통해 교대 근무 시간당 평균 15분을 단축하였다. 아울러 Park 등[A9]은 NVA 개선 활동으로 재입원 환자 안내 시간은 12분에서 9분, 물품 인수 인계 시간은 하루 평균 41.6분에서 21.5분으로 감소하였고, 물품 차용 건수는 211건에서 167건으로 줄었다. 이는 간호 업무의 비효율성을 개선하면 불필요한 시간을 줄이고 환자 및 간호사의 만족도를 향상시킬 수 있음을 보여 주었다.
논의
본 연구는 간호 업무 효율성과 관련된 NVA 활동과 NNT에 관한 25편의 연구를 분석하여, 국가별∙시기별 연구의 동향과 간호사의 직∙간접 업무, NVA 활동과 NNT의 유형과 특성, 각 업무의 개선이 간호 업무 효율성에 미치는 영향을 탐색하였다. 분석 결과, 2000년대 이후 국가별 의료 시스템의 유형에 따라 간호사의 역할 범위가 다르며, 의료 비용 절감과 인력 효율성 향상에 따라 NVA 활동과 NNT의 유형과 특성이 달랐다. 특히, NNT는 간호 소진, 환자의 안전과 간호의 질에 부정적인 영향을 미치며[
15], 간호사의 이직에도 영향을 주는 것으로 나타났다[
15,
24]. 비록 본 연구에서는 미완료 간호 또는 미완료 간호 업무를 다루지는 않았지만, 미완료 간호가 NNT와 유의한 상관관계를 보였다[
15,
16,
25-
27]. 미완료 간호 또는 미완료 간호 업무는 incomplete nursing tasks, missed nursing care, 또는 nursing care left undone 등으로 표현되며, 간호 업무 중 환자에게 필요한 간호가 근무 시간 내에 완료되지 않은 상태를 의미한다[
15,
16,
25-
27]. 이에 본 연구를 통해 간호사의 직∙간접 업무 외에 NVA 활동, NNT와 미완료 간호 업무와 관련된 연구 동향을 파악할 수 있었다.
NVA 활동과 NNT는 필수적∙본질적 간호 역할과 직접 관련이 낮으며, 불필요하거나 보조적인 성격을 지닌다. 따라서 간호 업무의 효율성 향상을 위해서는 직∙간접 간호, NVA 활동과 NNT소요 시간을 지속적으로 모니터링하는 것이 필요하다. 또한, 간호 임상현장에의 조직 구조, 인력 배치, 부서 간 업무 분배 형태에 따라 다양한 형태의 비효율적 간호 업무가 발생할 수 있으므로, 이를 규명하고 개선하는 과정이 선행되어야 한다. 이 과정에서 간호 보조 인력과 같이 비면허자가 수행 가능한 업무를 구분하여 관리해야 한다. 아울러 간호사의 업무 중 중첩되지만 환자의 안전과 생명에 직접적 영향을 미치지 않는 범위 내에서는 업무를 이관하고, 역할 조정을 통해 간호 업무 범위를 명확히 할 필요가 있다. 나아가 업무 협의 과정에서 발생할 수 있는 갈등을 최소화하기 위해 간호 조직 차원의 지원과 협력이 요구된다.
이에 업무 조정 방안으로 직•간접 간호를 제외하고 각 임상 단위별 업무, 개인적 활동, 문서 작업, 그리고 시간이 많이 소요되는 NVA 활동이나 NNT업무를 분류하거나[
9,
10], 간호 업무 중 반복, 중복, 대기, 타 분야 업무 대행, 업무 중단 후 재시작 등과 같은 NVA 활동을 기준으로 간호 요구도와 임상현장의 문제점을 분석하고 이를 줄이는 전략을 제시할 수 있다[
2,
10,
28]. 나아가 간호 업무를 세분화하여 의사 및 타 부서와의 의사소통, 투약, 장비 및 물품 관리, 기록, 검사, 입•퇴원 및 전동 등의 세부 항목으로 구분하거나[
11], 개선 가능성, 시급성, 경제성을 기준으로 분류하거나[
12], 환자 중심 간호 관점에서 primary work(환자 요구에 완전히 부합), secondary work (환자 요구와 부분적으로 관련), non-value-adding work (환자 요구와 무관)으로 구분하여[
29], 각 병원의 간호 단위의 특성에 맞게 반영, 활용할 필요가 있다[
15]. 비록 본 연구의 결과에 따라 업무 유형이 간호 임상 현장에서 관리•사무 업무, 환자 이송, 의사 업무 대행, 기타 의료 전문가 업무, 의사소통 및 조정 업무 등이 분류되었으나[
4] 임상현장에 따라 단순한 분류에 그치거나 의료현장의 변화에 따른 표준화된 업무 재분배와 모니터링이 부족한 실정이다. 이에 환자 중심의 간호 업무 효율성 향상을 위해, 임상 현장의 조직 구조와 인력 운영 등을 반영한 간호사의 직접간호, 필수 간호 업무 중심의 지속적인 재평가와 개선이 필요하다.
본 연구를 통해 직접 간호, 필수 간호 업무와 무관한 업무를 개선하면 직무 만족도[
28], 환자 만족도[
10], 교대 시간 단축[
15] 등에 긍정적인 영향을 미치는 것으로 나타났다. 그러나 일부 연구에서는 시스템 개선이 오히려 NVA 활동 시간을 증가시키거나[
10], 업무 유형을 재구성하고 간호 인력을 증원하더라도 필수 업무와 그 외 업무 간 소요 시간 비율은 크게 변하지 않는다는 결과도 보고되었다[
9,
30]. 이는 단순한 구조적 변화보다는 NVA 활동과 NNT를 구체적으로 파악하고 불필요한 업무를 줄이는 접근이 필요함을 시사한다[
9,
31,
32]. 특히, 환자 만족도를 높이기 위해 환자 사정, 교육, 심리적 안정 도모와 같은 직접 간호와 간호 조정∙관리 활동에 더 많은 시간을 할애해야 한다[
11,
12]. 이를 통해 간호사가 환자 안전과 간호 질 관리를 중심으로 업무를 수행할 수 있는 환경을 조성하는 것이 중요하다[
25,
33]. 또한 NVA 활동과 NNT를 통합적으로 관리하고 정기적으로 업무를 재구성함으로써 환자 중심 간호를 실현할 수 있는 방안을 모색할 필요가 있다[
9,
32].
NVA 활동과 NNT 발생 원인은 행정 시스템 지연[
10], 비효율적인 의사소통[
13], 인력 부족[
4], 제한된 자원[
31], 간호 관리 및 인식 부족[
15] 등으로 나타났다. 이는 필수 간호 업무 시간을 감소시키고 환자 안전과 간호 서비스 질에 부정적 영향을 미친다[
15,
16,
27,
33,
34]. 한편, Al-Kandari와 Thomas [
24]의 연구에서는 활동 기반 관리 접근을 통해 우선순위가 높은 간호 활동에 자원을 집중함으로써 환자 간호의 질을 향상시키고 비용을 절감할 수 있음을 보였다. 반면, NVA 활동과 NNT의 증가는 간호사의 직무 만족도 저하[
12], 근무 일정 유연성 감소[
15], 간호 업무 완성도 저하[
4]를 초래하였다. 이러한 문제를 해결하기 위해 NVA 활동과 NNT를 지속적으로 관리하고 각 유형별 항목을 조사하며 수정•보완하는 노력이 필요하다. 간호 보조 인력 및 의료 보조 인력의 적절한 활용과 병원 관리자의 적극적인 조정은 갈등을 최소화하고 신뢰 기반의 업무 환경을 조성하는 데 필수적이다[
2,
9,
15]. 또한, 적정 인력 배치 및 다학제적 협력을 통해 환자 중심의 간호 환경을 조성해야 한다[
4,
34]. 결론적으로, 간호사가 필수 간호에 더 많은 시간을 할애하고 환자 중심 간호를 실현할 수 있도록 NVA 활동과 NNT를 체계적으로 관리하고 정기적으로 평가하는 연구가 반복적으로 이루어져야 한다. 이러한 접근은 환자 안전과 간호의 질을 높이며, 의료 환경의 효율성과 지속 가능성을 동시에 강화할 것이다.
결론
본 연구는 간호사의 직•간접 간호 외에 NVA 활동과 NNT를 분석하여 업무 효율성을 향상시키며 간호 시간을 증진할 수 있는 방안을 탐색하였다. 연구 결과, 비효율적인 업무를 조정하고 환자 경험과 안전을 최우선으로 고려할 때 간호 업무 효율성이 향상되고 환자 중심의 간호 환경이 조성될 수 있음을 확인하였다. 이에 따라 본 연구는 NVA 활동과 NNT의 지속적인 관리와 재평가, 간호사의 역할 명확화와 업무 재구성을 통한 분업 체계 마련, 의료 시스템 개선을 통한 효율적 간호 환경 조성, 아울러 NVA 활동과 NNT가 간호사와 환자에게 미치는 영향을 심층적으로 분석하는 후속 연구의 필요성을 제언한다.
Article Information
-
Author contributions
Conceptualization: MHC. Methodology: MHC. Formal analy-sis: MHC, JHP, HB, MYJ. Data curation: MHC, YK, NYK, MJK, HJK, JHP, JIP, SYB, HB, EL, MYJ, SC. Visualization: MHC, MJK, JHP, HB, MYJ. Project administration: MHC, YK. Writing - origi-nal draft: MHC. Writing - review & editing: MHC, HB. All authors read and agreed to the published version of the manuscript.
-
Conflict of interest
None.
-
Funding
This study was supported by the Clinical Nursing Research Fund of Seoul National University Hospital in 2024 (Nursing Administration Education Team-667).
-
Data availability
Please contact the corresponding author for data availability.
-
Acknowledgments
None.
Figure 1.PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews: flow diagram for study selection process.
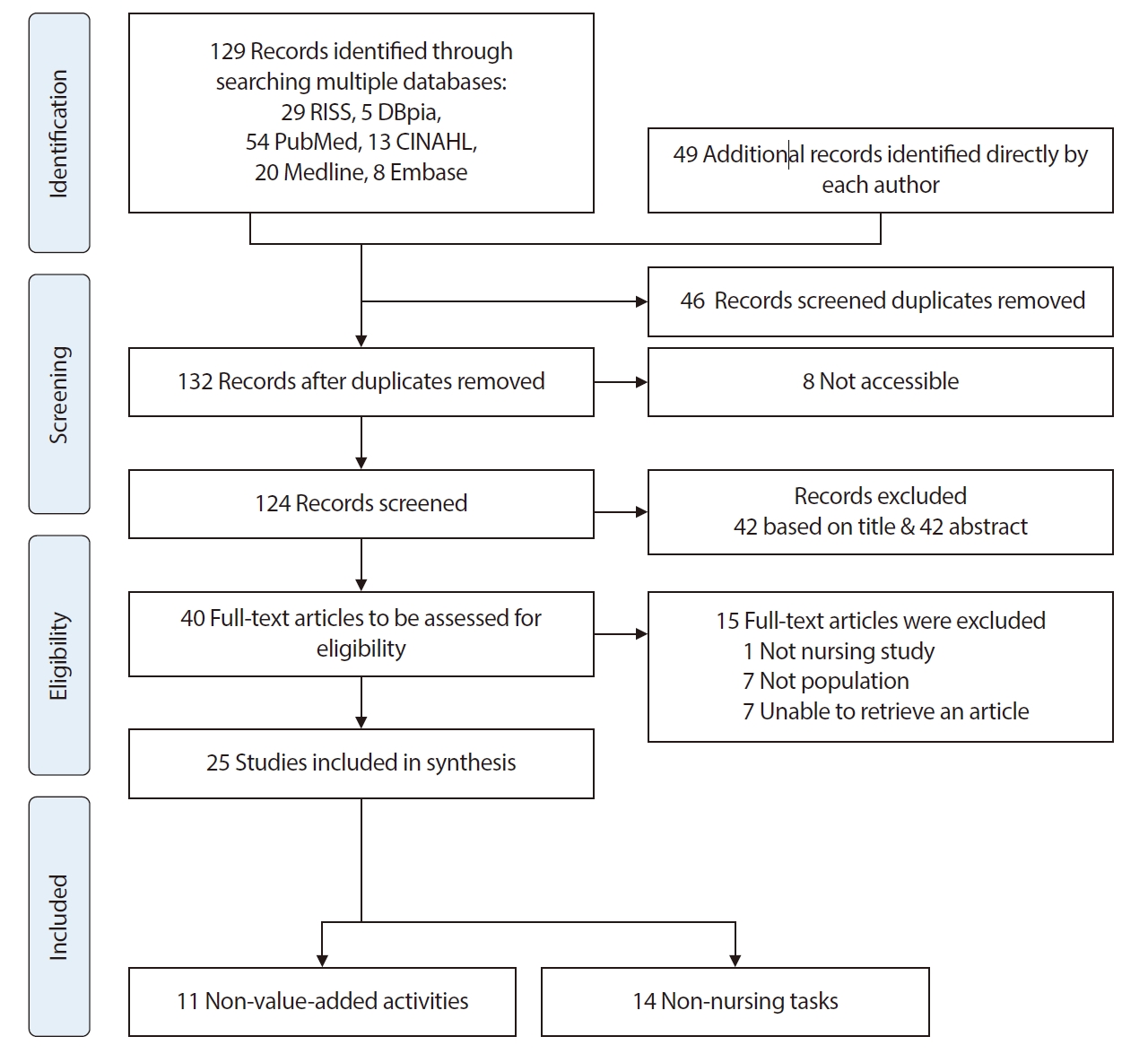
Table 1.General Characteristics of Literature (N=25)
|
Variable |
Category |
No. (%) |
|
|
NVA (n=11) |
NNT (n=14) |
Total |
|
Year of publication |
<2000 |
1 (9.1) |
0 |
- |
|
2000~2004 |
1 (9.1) |
2 (14.3) |
- |
|
2005~2009 |
4 (36.3) |
3 (21.4) |
- |
|
2010~2014 |
3 (27.3) |
0 |
- |
|
2015~2019 |
1 (9.1) |
4 (28.6) |
- |
|
2020~2024 |
1 (9.1) |
5 (35.7) |
- |
|
Journal of experimental research design |
Mixed method |
4 (36.4) |
1 (7.1) |
- |
|
Quantitative method |
5 (45.4) |
9 (64.3) |
- |
|
Qualitative method |
0 |
2 (14.3) |
- |
|
Feature |
1 (9.1) |
0 |
- |
|
Review article |
0 |
2 (14.3) |
- |
|
Case study |
1 (9.1) |
0 |
- |
|
Country |
United States |
6 (54.5) |
1 (7.1) |
- |
|
Korea |
4 (36.4) |
2 (14.3) |
- |
|
United Kingdom |
0 |
1 (7.1) |
- |
|
Others (Italy, Australia, Canada, Finland, Jordan, Egypt, Kuwait, South Africa) |
1 (9.1) |
10 (71.4) |
- |
|
Study on the place (n=22) |
Neuroscience - MS unit |
- |
- |
1 (4.5) |
|
MS unit |
- |
- |
12 (54.5) |
|
Surgical unit |
- |
- |
2 (9.1) |
|
Outpatient department |
- |
- |
1 (4.5) |
|
Other (L&D, integrated nursing care unit, ICU, ER, OR, etc.) |
- |
- |
6 (27.3) |
|
Type of participant (n=22) |
RN |
- |
- |
16 (72.7) |
|
Professional nurses |
- |
- |
1 (4.5) |
|
OPD RN |
- |
- |
1 (4.5) |
|
Others (LPN, UAP, technical partner, administrative partner and support partner etc.) |
- |
- |
4 (18.2) |
Table 2.Analysis of the Classification of Nursing Work: Value Added Activities (Direct and Indirect Care), Non-value-Added Activities, and Non-nursing Tasks
|
Major category |
Subcategory |
List of activity |
|
Value added activity |
|
|
|
Direct care |
Patient assessment and monitoring |
Assessing (monitoring, examinations) patient needs, patients’ status and (or) trends, vital signs, assess blood pressure, adequate patient surveillance, caring unstable patients and close monitoring, recording ECGs/managing deterioration of the clinical condition of the patient (not urgent or critical cases)/using clinical judgment/identifying needs (physical, mental, social, spiritual, financial), spiritual care |
|
Medication |
Administering medications (on time), medical services/IM injections, IV therapies and medications, oral medications, other medications |
|
Patient care treatments and technical skill |
Providing all treatments and procedures/communication with care team and relatives, provide patient information/respiratory care, tracheal suction, tracheostomy care/safety care/pain management/undertaking venipuncture, administering IV (insert IV), siting intravenous cannula, removing venflons/tube feeding/inserting NGT/catheter care (urinary catheterization)/making decisions about wound dressing, wound management, dressing changes/positioning (assistance with turning patient), frequent changing of patient position/transporting patient (prep/travel)/comfort care/comforting/talking with patient(s)/treat: hands-on technical care including personal care, procedures changes |
|
Nursing care planning |
Admission, discharge, discharge planning, preparing for discharge/planning, planning care, care planning tasks/preparing and updating nursing care plan, pathways (NCP), procedures/communication and explanation with patients and families (for planning care) |
|
Education and teaching |
Teaching and educating patients, family and (or) givers regarding disease, behavior changes, treatments, medications, care plan, client health teaching |
|
Daily activities and personal care |
Hygiene care, oral hygiene/all aspects of basic physical are associated with bathing, personal care bathing (complete partial)/skin care and pressure sore care, back rub/ADLs, grooming, ambulation/nutrition care, set up patient at mealtime, feeding, eating/elimination care/toileting/exercise/provide patient bedside procedures |
|
Emergency situations and critical care |
Life support/alarm/emergency, managing an urgent patient situation/performing extraordinary life support/assessing the newly admitted patents as an urgent case |
|
Delegation, management and supervision (delegable/patient care contacts) |
|
Indirect Care |
Communication and cooperation |
Communication with other providers care team and family/giving reports or shift report, reporting/sharing information with other care providers, collecting data from other units and departments (e.g., by calling) not appropriately recorded/information lookup/Working with orders, checking orders, processing doctor’s orders/processing laboratory orders and responses/psychosocial-assisting patients and (or) families understand and cope with psychosocial issue/related to patients’ transport, completion of transfers/care rounds, rounding/help others, supporting nursing tasks in favor of the patient(s) cared for by an inexpert colleague who has called supervision and advice (e.g., drainage care), providing tasks usually performed by the patient's caregiver(s)/coordination of care, coordination: collaborating, and facilitating service provision form a variety of services and disciplines including obtaining medications and supplies |
|
Documentation |
Write shift report/update care plans and documentation/review care plan and report/collecting data from the previous shift not appropriately transferred during handovers/recording patient status, orders and activities either on paper or electronically, EMR nursing record/chart/handoffs/adequate document nursing care/write out assignment |
|
Preparing |
Preparing equipment, documents, treatments, sampling, examinations |
|
Medication |
Preparing medications/medication activities, check medication, getting medication/medication rounds/computer (except for order transcription) |
|
Education and teaching |
Teaching/training and staff meetings/preceptor/care conferences |
|
Unit-related |
Equipment and supply management, supply – get, fill/prep, clean |
|
Others |
Gathering supplies (before treatment)/management of patient care, information, facility and patients’ belongings/travel time |
|
Non-value-added activities |
|
Personal |
|
Meals (lunch)/breaks, personal time/restroom/personal affairs include tasks such as adjusting personal schedules/socializing with coworkers/non-work-related activities/no contract |
|
Waste |
|
Other miscellaneous activities/other activities (not on the sheet)/external calls/trips outside the ward/checking equipment, it takes a lot of time to hand over equipment, goods etc. |
|
Interruption |
Interruptions (multiple ordering systems, multiple reports, providers per patient, non-patient related information) |
|
Searching |
Searching or retrieving things, person and equipment, looking for equipment, people and supplies because of shortage/borrowing medical instruments from other departments or words, borrowing equipment and materials/answering phone calls for confirmation or replying to irrelevant inquiries |
|
Waiting |
Waiting one's turn until others finish using the instrument or supplies/waiting for call, contact from another department/waiting for patient data to be entered into the system: physician orders not transferring with patients/waiting for porters who come late/waiting for the arrival of medicines for distribution, until arriving medicine or supplying materials, due to medication delivery delay from pharmacy/waiting until prescriptions are confirmed/waiting to obtain delayed order |
|
Reworking |
Repeating the measurement due to instrument failures, preparing and re-preparing the insufficient materials over again |
|
Delaying |
Delayed prescriptions, confirming prescription, placing a variety of orders/waiting for the delay, delayed start time/delay in supply of equipment, goods, etc. from supply department |
|
Repeating |
Trying repeatedly to call or to reach the attending physician, making repeated calls (to doctors, porters, etc.), telephone, repeats calls to staffing office (physicians)/having to make several calls to the patient or (his/her) guardian/having to visit the waiting room or patient's room repeatedly to check if the patient or their guardian has arrived/performing the process of works repeatedly due to the mistakes of doctors in the prescription/reconfirming orders due to error in prescriptions/unclear or inaccurate prescriptions/having to confirm frequently through the computer whether doctors make out the prescriptions |
|
Duplicating |
Repeating meaningless measurements and recording them over again |
|
Documentation |
All activities associated with documenting |
Charting, documenting nursing care delivered, paper records, computer data entry, the action of documenting, recording actual treatment, managing the clinical, administrative paperwork, medications’ paperwork, admission and discharge paperwork, other documentation, unnecessary paperwork/writing care plan/transcribe orders /email and text paging |
|
Duplicating |
Documenting the double records |
|
Repeating |
Repetition or duplication of nursing records |
|
Patient review and evaluation |
Locating charts/reviewing and charting (HER, paper), evaluating patient’s condition and care (including the review of all patient data)/searching for results (locating reports, working on the computer terminals, paper records) |
|
Reworking |
Computer downtime, lack of interface between systems and problems, complex EMR system/entering data over again due to the computer crash during the data entering, re-entering data owing to the computer crashing process of entering data/entering written data (or handwritten) into the computer |
|
Waiting |
Waiting until the computer is functioning (rebooting after login, slow speed) |
|
Repeating |
Repeated calls due to incomplete medical certification and documents |
|
Searching |
Taking much time to find educational materials (including both data saved on the computer and written documents) |
|
Necessary activities |
Admission process |
Admission/missing meals during late admission/it takes a lot of time to research nursing information for short-term hospitalized patients/excessive call volume from the care team regarding hospitalization time/bed placement/calls between wards upon admission to other departments |
|
Waiting |
Waiting or confirming bed preparation for admission |
|
Reworking |
Repeating simple jobs such as orientation on admission/guide to repeated hospitalization for readmitted patients |
|
Repeating |
Calling the admission office regarding bed assignment, appointment, documents |
|
Delaying |
Delay in hospitalization information due to simultaneous hospitalization |
|
Discharge process |
Missing meals when discharge is canceled, difficulty explaining necessary items after discharge, missing information on patient needs (outpatient schedule and discharge medication), inconvenience in scheduling a test after discharge, inconvenient explanation using discharge plan/discharge/multiple calls for transport |
|
Waiting |
Waiting for the completion of transfers |
|
Repeating |
Repeated calls for transfer, delays in completion of transfers |
|
Diagnostic and test procedures |
Whether or not a central venous line is used in the laboratory varies/discrepancies in patient and nurse education materials/telephone service related to CVR results and test prescriptions/writing the wrong consent form/missing samples/scheduling laboratory, radiology, and other diagnostic tests |
|
Reworking |
Rescheduling test time, confirming specimen requisitions |
|
Repeating |
Repeated calls for appointment, rescheduling of follow-up diagnostic tests |
|
Indirect care |
Paging care team, calling ancillary staff and (or) care team, coordinating ancillary services/searching for auxiliary staff and care team/difficulty applying labels to people at high risk of falling/Requiring tasks not provided by the medical team (e.g, asking again for pain medication)/escorting patients, related to patient transport/organizing outpatient care/doing nursing tasks (e.g., drainage care) in a supernumerary patient/central venous management takes a lot of time, handling time required for central venous line management/delivering supplies, delivering and retrieving food trays, ordering, coordinating and performing ancillary services, dietary services (delivering and retrieving food trays) |
|
Repeating |
Passing the information or messages to doctors from other departments (laboratory, radiology, insurance review, pharmacy, etc.)/delivering information between care teams, delivering test results to physicians/repeating the calls to the proper person or department for favors, replies and confirmations (doctors, pharmacy, laboratory, etc.)/making repeated the calls to the concerned person or department for favors, replies and confirmations/repeatedly making calls to other departments to get an update on the situation, making contact calls repeatedly to appreciate the situation in other departments or wards/reconfirming or re-coordinating work due to lack of communication & collaboration between attending physicians, medical interns, and collaborating physicians/obtaining needed information (some explanation added) from other departments (other wards, pharmacy or admission and discharge department) |
|
Searching |
Returning to the station to get needed articles during making a round to the patient's room |
|
Duplicating |
Double assessments and work being done twice (handing/taking over the duty both verbally and through the computer) |
|
Waiting |
Waiting times required to integrate the process of nursing care with other processes (e.g, medical, diagnostic)/waiting for patients or the results of joint treatments |
|
Reworking |
Repetitive confirmation due to miscommunication with other departments/returning to the station to answer the phone calls from other departments and resuming the interrupted work caused by other urgent work or the prescription |
|
Reverse-Proxy Working |
Frequent checks for their proper function (doctor, pharmacy, nutrition department)/compensating tasks not provided by secretaries/handling the works for doctors/Providing information to not seeing patients/handling the works for the nutrition department (removing the food plate to the tray, diet consultation, dietary education)/optional meal application many missing |
|
Medication |
Dispenser, malfunctioning dispensers, completing paperwork for missing dispenser, delayed responses for now orders, inability to haver new pharmacy orders – requiring nurses to leave the unit to obtain the medication/receiving pharmacy, going frequently to the pharmacy to get medicines, making frequent trips to the pharmacy for medicines |
|
Reverse-Proxy Working |
Handling the work for the pharmacy department (advice on medicines, producing educational materials, identifying and controlling medicines, self-medications) |
|
Duplicating |
Having to sort out the prescribed medicines by room and patient/returning medications, complicated medication return process when a patient dies at night |
|
Unit-related |
Administrative activities |
Arranging for ambulance/changing nurse assignments, staffing changes/rearranging assignments mid-shift/staff meetings, attending meeting/departmental tasks/calls between wards upon admission to other departments/time loss because of changing teams/request to repair equipment, ordering supplies/Searching for necessary items |
|
Reverse-Proxy Working |
Delivering in person the failed instruments to the proper department/delivering failed instruments to the proper department in person |
|
Reworking |
Resetting the instrument which has been applied to other patients |
|
Cleaning |
Cleaning equipment/cleaning, housekeeping, general housekeeping (such as indent for store, maintenance, electro, plumb), warehouse tasks, food supply, maintenance of equipment |
|
Management and supervision |
Work supervision, providing supervision to nursing aides/compensating tasks not provided by the nursing aides/managing an unexpected rise in patient volume/cooperation with other wards/training, student education, counselling, employee orientation, supervising novice colleagues in their first period of introduction in the unit, in-service education/managing tension or communication breakdowns with nursing aides, nursing staff and medical staff |
|
Non-nursing tasks |
|
Admission and discharge |
Admission, transfers and discharge, arranging discharge and transportation (including to long-term care)/transport of patients, transporting patients, transporting of patients within hospital, escorting patients, pottering duties |
|
Equipment |
Equipment, obtaining supplies or equipment (from other units), maintenance of supplies/searching for and retrieving equipment |
|
Documentation |
Replenish charts and forms, processing documents/records transfer and copying/tidying medical records takes |
|
Waste |
Answering telephones, call bell/searching for people |
|
Administrative activities |
Rounding errands/planning appointments/clerical duties-general, management and clerical tasks, administrative activities (ordering, printing)/scheduling meetings not regarding patients, as a secretary/performing auxiliary services/ordering, coordinating and performing ancillary services |
|
Reverse-proxy working |
Routine phlebotomy, blood drawing for tests/other duties such as receiving pharmacy or arranging for ambulance/filling in for non-nursing services (or care) not available off-hours, performing non-nursing care/housekeeping duties, domestic duties |
|
Cleaning |
Cleaning patients’ rooms and equipment, maintenance of hygienic environment, tidying up room, emptying trash bins/make beds, gather linen, receiving linen |
|
Others |
Delivering and retrieving trays/distributing lunch trays |
Table 3.Analysis of Nursing Work Efficiency According to Research Main Outcomes
|
Category |
List of activities |
Capuano et al. (2004) [A2] |
Upenieks et al. (2007) [A3] |
Desjardins et al. (2008) [A14] |
Park et al. (2013) [A9] |
|
– |
NC |
+ |
– |
NC |
+ |
– |
NC |
+ |
– |
NC |
+ |
|
Direct care time |
|
√ |
|
|
√ |
|
|
|
|
|
|
|
|
|
Assessment/monitoring |
√ |
|
|
|
|
|
|
|
|
|
|
|
|
Medication care |
|
|
|
|
|
|
|
|
|
|
|
|
|
Admission |
|
|
|
|
|
|
|
|
|
√ |
|
|
|
Transfer |
√ |
|
|
|
|
|
|
|
|
|
|
|
|
Discharge |
√ |
|
|
|
|
|
|
|
|
|
|
|
|
Indirect care time |
|
|
|
√ |
√ |
|
|
√ |
|
|
√ |
|
|
|
Documentation |
|
√ |
|
|
|
|
√ |
|
|
|
|
|
|
|
Quality indicators |
Falls |
√ |
|
|
|
|
|
|
|
|
|
|
|
|
Nosocomial ulcer |
|
|
√ |
|
|
|
|
|
|
|
|
|
|
Restraint use |
|
|
√ |
|
|
|
|
|
|
|
|
|
|
Medical error |
|
|
|
|
|
|
|
|
|
|
|
|
|
Value added |
|
|
|
√ |
|
|
|
|
|
|
|
|
|
Non-value added |
|
|
|
|
|
√ |
|
|
|
√ |
|
|
|
Patient satisfaction |
|
|
|
|
|
|
|
|
|
|
|
√ |
|
Turnover time |
√ |
|
|
|
|
|
√ |
|
|
√ |
|
|
|
Employee satisfaction |
|
|
√ |
|
|
|
|
|
|
|
|
√ |
|
Job functions and roles |
|
|
√ |
|
|
|
|
|
|
|
|
|
|
Nursing tasks left undone |
|
|
|
|
|
|
|
|
|
|
|
|
REFERENCES
- 1. Lee SK. A study on the role of patient experience to enhance co-creation of healthcare service. Global Business Administration Review. 2021;18(6):131-151.
- 2. Choi JS, Yang YH, Baek HS. Types and causes of non-value-added activities in nursing practice in Korea. Journal of Korean Clinical Nursing Research. 2011;17(3):363-374.
- 3. Grosso S, Tonet S, Bernard I, Corso J, De Marchi D, Dorigo L, et al. Non-nursing tasks as experienced by nurses: a descriptive qualitative study. International Nursing Review. 2019;66(2):259-268. https://doi.org/10.1111/inr.12496
- 4. Aldarawsheh AA, Saifan AR, Sawalha MA, Assaf EA, Alrimawi I, Elshatarat RA, et al. Exploring the causes and consequences of non-nursing tasks among nurses in Jordan: an in-depth qualitative investigation. Applied Nursing Research. 2024;77:151791. https://doi.org/10.1016/j.apnr.2024.151791
- 5. Winner L, Reinhardt E, Benishek L, Marsteller J. Lean management systems in health care: a review of the literature. Quality Management in Health Care. 2022;31(4):221-230. https://doi.org/10.1097/QMH.0000000000000353
- 6. Upenieks VV, Akhavan J, Kotlerman J, Esser J, Ngo MJ. Value-added care: a new way of assessing nursing staffing ratios and workload variability. JONA: The Journal of Nursing Administration. 2007;37(5):243-252. https://doi.org/10.1097/01.NNA.0000269744.17266.47
- 7. Murman E, Allen T, Bozdogan K, Cutcher-Gershenfeld J, McManus H, Nightingale D, et al. Lean enterprise value: insights from MIT’s lean aerospace initiative. Neoflux, translator. Seoul: Gasan Publishing; 2008.
- 8. Ohno T. Toyota production system: beyond large-scale production. Kim HY, translator. Seoul: Mirae Publishing; 2004.
- 9. Capuano T, Bokovoy J, Halkins D, Hitchings K. Work flow analysis: eliminating non-value-added work. The Journal of Nursing Administration. 2004;34(5):246-256. https://doi.org/10.1097/00005110-200405000-00008
- 10. Storfjell JL, Omoike O, Ohlson S. The balancing act: patient care time versus cost. The Journal of Nursing Administration. 2008;38(5):244-249. https://doi.org/10.1097/01.NNA.0000312771.96610.df
- 11. Kim MY, Park SA. Study on non-value-added nursing activities in a tertiary hospital. Journal of Korean Academy of Nursing Administration. 2011;17(3):315-326. https://doi.org/10.11111/jkana.2011.17.3.315
- 12. Park YH, kwon IG, Park KS, Jang HJ, Song MR, Kim HJ. Case study on improvements in non-value-added nursing activities to increase the efficiency of nursing care. Quality Improvement in Health Care. 2013;19(2):68-80. https://doi.org/10.14371/QIH.2013.19.2.068
- 13. Upenieks VV, Akhavan J, Kotlerman J. Value-added care: a paradigm shift in patient care delivery. Nursing Economic. 2008;26(5):294-300.
- 14. Pearson A. Multidisciplinary nursing: re-thinking role boundaries. Journal of Clinical Nursing. 2003;12(5):625-629. https://doi.org/10.1046/j.1365-2702.2003.00794.x
- 15. Park JY, Hwang JI. Relationships among non-nursing tasks, nursing care left undone, nurse outcomes and medical errors in integrated nursing care wards in small and medium-sized general hospitals. Journal of Korean Academy of Nursing. 2021;51(1):27-39. https://doi.org/10.4040/jkan.20201
- 16. Al-Kandari F, Thomas D. Factors contributing to nursing task incompletion as perceived by nurses working in Kuwait general hospitals. Journal of Clinical Nursing. 2009;18(24):3430-3440. https://doi.org/10.1111/j.1365-2702.2009.02795.x
- 17. Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, et al. Nurses' reports on hospital care in five countries. Health Affairs. 2001;20(3):43-53. https://doi.org/10.1377/hlthaff.20.3.43
- 18. Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, et al. Prevalence, patterns and predictors of nursing care left undone in European hospitals: results from the multicountry cross-sectional RN4CAST study. BMJ Quality and Safety. 2014;23(2):126-135. https://doi.org/10.1136/bmjqs-2013-002318
- 19. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19-32. https://doi.org/10.1080/1364557032000119616
- 20. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine. 2018;169(7):467-473. https://doi.org/10.7326/M18-0850
- 21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71
- 22. Eldawlatly A, Alshehri H, Alqahtani A, Ahmad A, Al-Dammas F, Marzouk A. Appearance of population, intervention, comparison, and outcome as research question in the title of articles of three different anesthesia journals: a pilot study. Saudi Journal of Anaesthesia. 2018;12(2):283-286. https://doi.org/10.4103/sja.SJA_767_17
- 23. Zepeda-Lugo C, Tlapa D, Baez-Lopez Y, Limon-Romero J, Ontiveros S, Perez-Sanchez A, et al. Assessing the impact of lean healthcare on inpatient care: a systematic review. International Journal of Environmental Research and Public Health. 2020;17:(15):5609. https://doi.org/10.3390/ijerph17155609
- 24. Al-Kandari F, Thomas D. Perceived adverse patient outcomes correlated to nurses' workload in medical and surgical wards of selected hospitals in Kuwait. Journal of Clinical Nursing. 2009;18(4):581-590. https://doi.org/10.1111/j.1365-2702.2008.02369.x
- 25. Bekker M, Coetzee SK, Klopper HC, Ellis SM. Non-nursing tasks, nursing tasks left undone and job satisfaction among professional nurses in South African hospitals. Journal of Nursing Management. 2015;23(8):1115-1125. https://doi.org/10.1111/jonm.12261
- 26. Palese A, Bottega M, Cescutti A, Caruzzo D, Danielis M, Fabris S, et al. Depicting clinical nurses' priority perspectives leading to unfinished nursing care: a pilot Q methodology study. Journal of Nursing Management. 2020;28(8):2146-2156. https://doi.org/10.1111/jonm.13036
- 27. Hammad M, Guirguis W, Mosallam R. Missed nursing care, non-nursing tasks, staffing adequacy, and job satisfaction among nurses in a teaching hospital in Egypt. Journal of the Egyptian Public Health Association. 2021;96:(1):22. https://doi.org/10.1186/s42506-021-00083-0
- 28. Song KJ, Kim EH, Yoo CS, Park HO, Park GO. Development of KPCS (Korean Patient Classification System for Nurses) based on nursing needs. Journal of Korean Clinical Nursing Research. 2009;15(1):5-17. https://doi.org/10.22650/JKCNR.2009.15.1.5
- 29. Michelman JE, Rausch PE, Barton TL. Value measurement in health care: a new perspective. Healthcare Financial Management. 1999;53(8):48-53.
- 30. Ha MK, Kim DH. The types and causative factors of non-value-added nursing activities in outpatient departments. Global Health and Nursing. 2022;12(1):57-68. https://doi.org/10.35144/ghn.2022.12.1.57
- 31. Storfjell JL, Ohlson S, Omoike O, Fitzpatrick T, Wetasin K. Non-value-added time: the million dollar nursing opportunity. JONA: The Journal of Nursing Administration. 2009;39(1):38-45. https://doi.org/10.1097/NNA.0b013e31818e9cd4
- 32. Desjardins F, Cardinal L, Belzile E, McCusker J. Reorganizing nursing work on surgical units: a time-and-motion study. Nursing Leadership. 2008;21(3):26-38. https://doi.org/10.12927/cjnl.2008.20057
- 33. Antinaho T, Kivinen T, Turunen H, Partanen P. Nurses' working time use: how value adding it is? Journal of Nursing Management. 2015;23(8):1094-1105. https://doi.org/10.1111/jonm.12258
- 34. Grosso S, Longhini J, Tonet S, Bernard I, Corso J, de Marchi D, et al. Prevalence and reasons for non-nursing tasks as perceived by nurses: findings from a large cross-sectional study. Journal of Nursing Management. 2021;29(8):2658-2673. https://doi.org/10.1111/jonm.13451
Appendix
Appendix 1.
Studies Included in Scoping Review
A1. Michelman JE, Rausch PE, Barton TL. Value measurement in health care: a new perspective. Healthcare Financial Management. 1999;53(8):48-53.
A3. Upenieks VV, Akhavan J, Kotlerman J, Esser J, Ngo MJ. Value-added care: a new way of assessing nursing staffing ratios and workload variability. JONA: The Journal of Nursing Administration. 2007;37(5):243-252.
https://doi.org/10.1097/01.NNA.0000269744.17266.47
A5. Upenieks VV, Akhavan J, Kotlerman J. Value-added care: a paradigm shift in patient care delivery. Nursing Economic. 2008;26(5):294-300.
A6. Storfjell JL, Ohlson S, Omoike O, Fitzpatrick T, Wetasin K. Non-value-added time: the million dollar nursing opportunity. JONA: The Journal of Nursing Administration. 2009;39(1):38-45.
https://doi.org/10.1097/NNA.0b013e31818e9cd4
A7. Choi JS, Yang YH, Baek HS. Types and causes of non-value-added activities in nursing practice in Korea. Journal of Korean Clinical Nursing Research. 2011;17(3):363-374.
A9. Park YH, kwon IG, Park KS, Jang HJ, Song MR, Kim HJ. Case study on improvements in non-value-added nursing activities to increase the efficiency of nursing care. Quality Improvement in Health Care. 2013;19(2):68-80.
https://doi.org/10.14371/QIH.2013.19.2.068
A10. Antinaho T, Kivinen T, Turunen H, Partanen P. Nurses' working time use: how value adding it is? Journal of Nursing Management. 2015;23(8):1094-1105.
https://doi.org/10.1111/jonm.12258
A14. Desjardins F, Cardinal L, Belzile E, McCusker J. Reorganizing nursing work on surgical units: a time-and-motion study. Nursing Leadership. 2008;21(3):26-38.
https://doi.org/10.12927/cjnl.2008.20057
A16. Al-Kandari F, Thomas D. Perceived adverse patient outcomes correlated to nurses' workload in medical and surgical wards of selected hospitals in Kuwait. Journal of Clinical Nursing. 2009;18(4):581-590.
https://doi.org/10.1111/j.1365-2702.2008.02369.x
A17. Bekker M, Coetzee SK, Klopper HC, Ellis SM. Non-nursing tasks, nursing tasks left undone and job satisfaction among professional nurses in South African hospitals. Journal of Nursing Management. 2015;23(8):1115-1125.
https://doi.org/10.1111/jonm.12261
A19. Yen PY, Kellye M, Lopetegui M, Saha A, Loversidge J, Chipps EM, et al. Nurses' time allocation and multitasking of nursing activities: a time motion study. America Medical Informatics Association Annual Symposium Proceeding Archive. 2018:2018;1137-1146.
A20. Grosso S, Tonet S, Bernard I, Corso J, De Marchi D, Dorigo L, et al. Non-nursing tasks as experienced by nurses: a descriptive qualitative study. International Nursing Review. 2019;66(2):259-268.
https://doi.org/10.1111/inr.12496
A21. Palese A, Bottega M, Cescutti A, Caruzzo D, Danielis M, Fabris S, et al. Depicting clinical nurses' priority perspectives leading to unfinished nursing care: a pilot Q methodology study. Journal of Nursing Management. 2020;28(8):2146-2156.
https://doi.org/10.1111/jonm.13036
A22. Grosso S, Longhini J, Tonet S, Bernard I, Corso J, de Marchi D, et al. Prevalence and reasons for non-nursing tasks as perceived by nurses: findings from a large cross-sectional study. Journal of Nursing Management. 2021;29(8):2658-2673.
https://doi.org/10.1111/jonm.13451
A23. Hammad M, Guirguis W, Mosallam R. Missed nursing care, non-nursing tasks, staffing adequacy, and job satisfaction among nurses in a teaching hospital in Egypt. Journal of the Egyptian Public Health Association. 2021;96(1):22.
https://doi.org/10.1186/s42506-021-00083-0
A24. Park JY, Hwang JI. Relationships among non-nursing tasks, nursing care left undone, nurse outcomes and medical errors in integrated nursing care wards in small and medium-sized general hospitals. Journal of Korean Academy of Nursing. 2021;51(1):27-39.
https://doi.org/10.4040/jkan.20201
A25. Aldarawsheh AA, Saifan AR, Sawalha MA, Assaf EA, Alrimawi I, Elshatarat RA, et al. Exploring the causes and consequences of non-nursing tasks among nurses in Jordan: an in-depth qualitative investigation. Applied Nursing Research. 2024;77:151791.
https://doi.org/10.1016/j.apnr.2024.151791
 , Youngah Kim2
, Youngah Kim2 , Na Yeong Kim3
, Na Yeong Kim3 , Min Ju Kim3
, Min Ju Kim3 , Hyeon Jin Kim3
, Hyeon Jin Kim3 , Ju Hee Park3
, Ju Hee Park3 , Ji In Park3
, Ji In Park3 , Su Yeon Bae3
, Su Yeon Bae3 , Heajin Bae3
, Heajin Bae3 , Eunjeong Lee3
, Eunjeong Lee3 , Min Young Jeon3
, Min Young Jeon3 , Suyoung Choi3
, Suyoung Choi3